Dedicated to Preventing and Treating Childhood Health Issues
A leader in fostering healthy lifestyles, the center is dedicated to disseminating the latest knowledge regarding pediatric healthy lifestyles, from its biological origins to its societal impact.
The center focuses on five key areas: education, research, advocacy, community, and clinical.
Welcome to the Center for Children's Healthy Lifestyles & Nutrition
Our primary goal is to contribute new knowledge regarding pediatric healthy lifestyles, ranging in scope from its biological origins to its societal impact. Current studies are exploring physiology, cognition, behavior, physical activity, and nutrition as they relate to many child health issues including obesity and diabetes, with a strong focus on energy metabolism disruption.
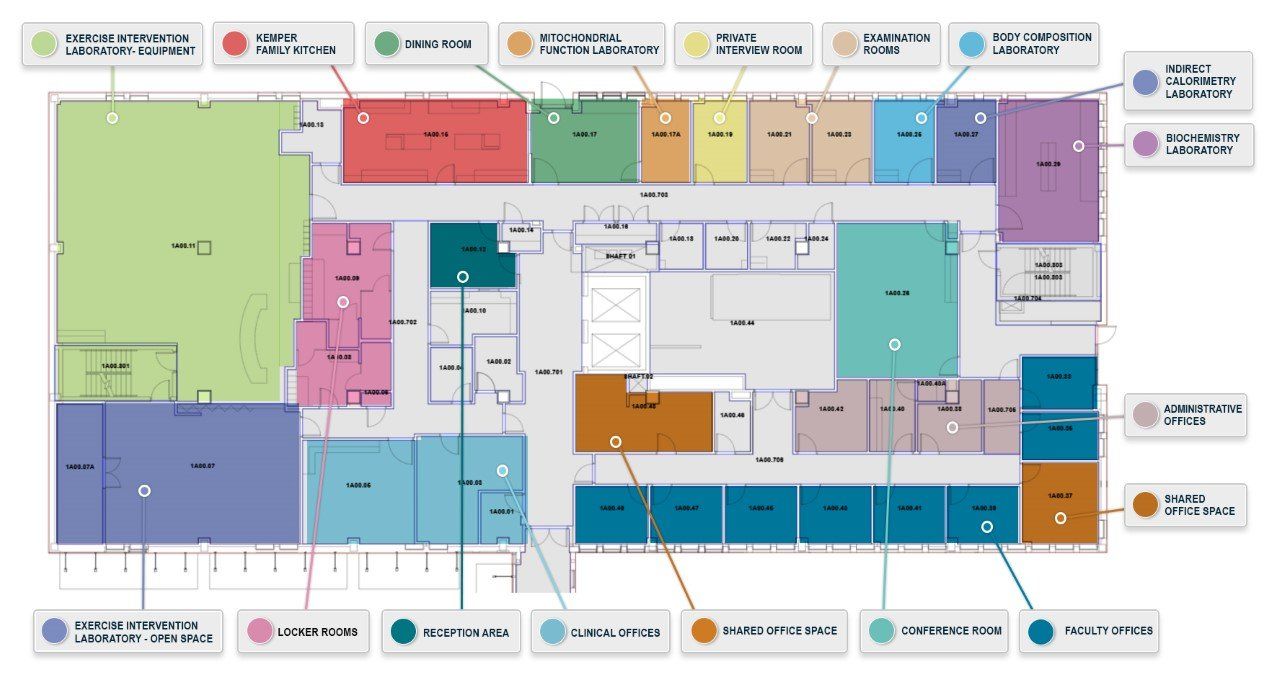
Our Building
The Center for Children’s Healthy Lifestyles & Nutrition is located on the first floor of the Donald Chisholm Building on the campus of Children’s Mercy Kansas City. The Center is a 14,000-square-foot facility designed to support clinical and bench research, individual clinical and group educational interventions, as well as offices for faculty and research staff.
The Center’s 800-square-foot demonstration kitchen features four prep stations, each with a GE Profile refrigerator and microwave. The kitchen contains four oven/stove/exhaust hood combinations and two dishwashers. The 500-square-foot wet lab features extensive countertop space, an exhaust hood and a -80 degree freezer. Testing rooms contain an indirect calorimeter, treadmill and DEXA. Clinical exam rooms and a waiting room are also available. The Center’s 2400-square-foot exercise facility features treadmills, stationary bicycles, elliptical trainers and weight machines, and has a large area for group physical activity. Locker rooms, showers and laundry facilities are also available. The Center provides conference room facilities for 10-50 attendees.
Please read our Center Use Guidelines. If you are interested in using space at the Center, please complete this
application. Once it’s submitted, it will be reviewed by the leadership team, and someone will respond within 10 business days.
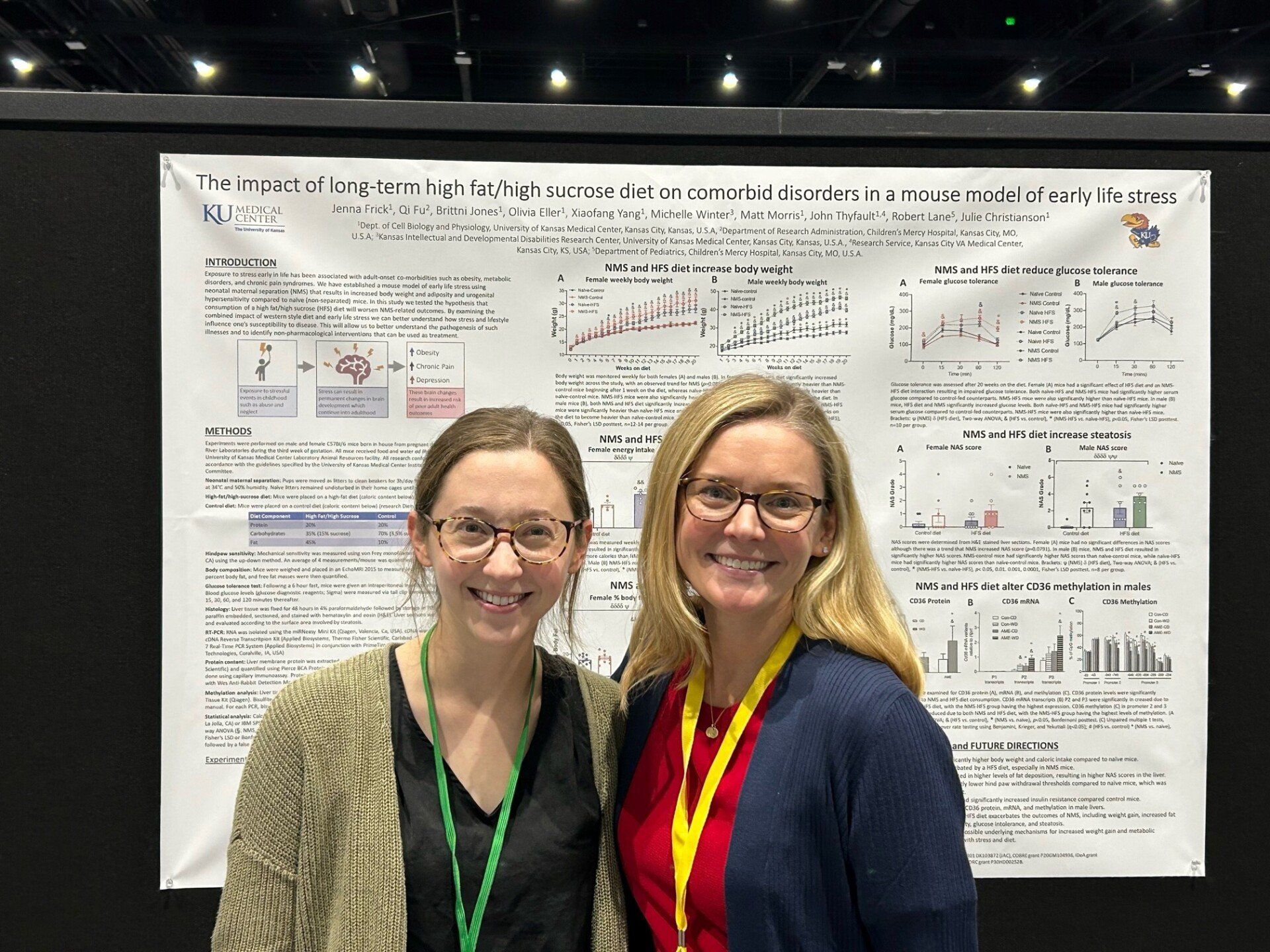
Gallery
-
City skyline
Photo By: John DoeButton